- Posted on
Addiction and ADHD
Attention deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder, which often prevails throughout an individual’s life. ADHD has various comorbidities, one of them being Substance Abuse (SA). SA is not a disorder but can lead to one – Substance Use Disorder (SUD), in the case of long-term drug consumption leading to dependency, both psychological and physical. Learning about this comorbidity is important, since ADHD is relatively prevalent, as are deaths from substance use and overdose.
Teenagers with ADHD are more likely to engage in substance abuse. During their rapid development, adolescence is known to engage in risky, potentially harmful development for many reasons, including family influences, peer pressure, and simple curiosity. While teenagers and adults with ADHD are twice as likely to develop a nicotine dependency via smoking, this further leads them to a higher risk of consuming alcohol (ethanol) or other substances later on. Overall, in comparison to the general population, those with ADHD are at a higher risk of SA and show a higher duration of active dependency.
Interestingly, more research has found that abuse of specific substances is associated with different symptoms prevailing in a person with ADHD. Someone who struggles more with hyperactivity, for example, tends to abuse cocaine and nicotine above all substances.

While we can never generalize the causes of mental disorder comorbidities, there are some theories on why those with ADHD often struggle with SUD. In addition to explanations of SA in adolescence above, they also often explain their abuse as means to reduce emotionality or attempts to aid their sleep. The explanations are dependent on the drug of choice. Adults, for example, report higher executive function and enhanced attention when using nicotine. Some research explains the causes through personality. Davis et al. (2015) identified a “high-risk personality” consisting of impulsivity, reward drive, neuroticism, and anxious tendencies. While Waluk et al. (2016) linked both disorders to a type B personality: easy-going, energetic, and flexible. Further influences include genetics and neurobiological development. While both SUD and ADHD are heritable, Weissenberger et al. (2017), note that they share a genetic pathway and a dopamine receptor, associated with both addiction and ADHD. Moreover, a portion of specific brain abnormalities, associated with impulsivity, reward sensitivity, and lack of control; overlap between the two disorders.
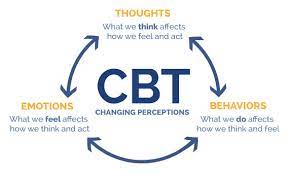
While ¼ of those with ADHD also struggle with SUD, their prognosis is significantly less positive due to the complexity of the comorbidity. Researchers stress the fact that it is important to tackle the issue from early on, to prevent substance us extending into adulthood. Moreover, it is important to develop a range of alternative coping mechanisms (Molina and Pelham, 2014), so one does not turn to substances in a stressful situation. Despite some research emphasizing the occurrences of stimulant abuse in those with ADHD, it has majorly been shown that early exposure to stimulants (prevalent ADHD treatment), lessens the risk of substance use (Schellekens et al., 2020). Finally, it has also been suggested to make use of integrative therapies, specifically based on Cognitive Behavior Therapy, focused on issues of both ADHD and SUD.
In conclusion, just like with most comorbidities, the link between ADHD and SUD or SA is complex. There is a vast amount of research on its prevalence and possible influences or causes. However, the treatment prospectives call for more exploration and the development of comorbidity-specific therapy.
by Diana Sultanova, Mental Health Intern
References
Davis, C., Cohen, A., Davids, M., & Rabindranath, A. (2015). Attention-deficit/hyperactivity disorder in relation to addictive behaviors: a moderated-mediation analysis of personality-risk factors and sex. Frontiers in psychiatry, 6, 47. https://doi.org/10.3389/fpsyt.2015.00047
Schellekens, A. F. A., van den Brink, W., Kiefer, F., & Goudriaan, A. E. (2020). Often Overlooked and Ignored, but Do Not Underestimate Its Relevance: ADHD in Addiction – Addiction in ADHD. European addiction research, 26(4-5), 169–172. https://doi.org/10.1159/000509267
Weissenberger, S., Ptacek, R., Klicperova-Baker, M., Erman, A., Schonova, K., Raboch, J., & Goetz, M. (2017). ADHD, Lifestyles and Comorbidities: A Call for an Holistic Perspective – from Medical to Societal Intervening Factors. Frontiers in psychology, 8, 454. https://doi.org/10.3389/fpsyg.2017.00454